Seeing the full picture of a horse’s body from the inside began not with a hoof, but with a woman’s hand. The accidental discovery of the radiograph in 1895 by the German physicist Wilhelm Conrad Röntgen transformed the human medical landscape. Still another century passed before advancements in equine diagnostic imaging revolutionized veterinary medicine.
X-Rays and Ultrasound
Early radiographs (X-rays), while groundbreaking for both human and equine medicine, rendered complications. The analog film required wet processing and often lacked sufficient image detail and quality. Delays between image development and delivery to medical professionals impeded swift diagnoses. However, with the advent of portable digital machines, equine practitioners can now capture high-quality images of bone at a horse’s stall rather than in a veterinary clinic.

Later, ultrasound technology came onto the scene, employing high-frequency sound waves to produce high-resolution, two-dimensional images of tendons and ligaments. With the ultrasound, veterinarians can assess soft-tissue injuries, colic, pregnancy, and suspicious masses, such as abscesses and tumors. Advanced speed and the accuracy of high-resolution, two-dimensional images improve physical exams.
CT and MRI
Equine diagnostic imaging rocketed to the next chapter with the introduction of CT and MRI in the 1990s, according to Katherine Garrett, DVM, Dipl. ACVS, director of diagnostic imaging at Rood and Riddle Equine Hospital in Lexington, Ky.
“The most significant change in equine diagnostic imaging is the widespread adoption of cross-sectional imaging modalities,” she says. “Their introduction allows us to make much more specific diagnoses than we could previously and understand different diseases more thoroughly.”

The difference between the traditional X-ray and a CT scanner lies in the type of image. A CT scanner examines slices of bone and soft-tissue structures on multiple planes from multiple angles and is beneficial for diagnosing cases of lameness and sinus, dental, and neurological issues.
Traditional CT scans performed on a fully anesthetized and recumbent horse presented its share of risks. The standing CT scans lower legs and images the head and neck. Because the horse only requires mild sedation, fewer complications and threats to the horse and the clinician occur.
Sarah Puchalski, DVM, Dipl. ACVR, head of Diagnostic Imaging at Palm Beach Equine Clinic in Wellington, Fla., cautions horse owners to understand how different types of image qualities vary between scanners.
“There is a difference in image quality for CT scanners, and what can and cannot be scanned,” she says. “CT is used for dentition in the skull and fracture evaluation. Soft tissue detail isn’t as good as the MRI, but the bone detail is superior.”
Soft-tissue injuries present a puzzle, especially in cases of lameness. MRI, first performed on horses in the late 1990s, benefitted from early clinical use but shot to the top of imaging modalities in the past five years. Today, MRI is considered the gold standard of diagnostic imaging for soft tissue and orthopedic injuries by using magnetic fields and radiofrequency pulses to generate images.

Puchalski notes that the particular benefit of the MRI rests in diagnosing the source of lameness.
“For example, inside the hoof capsule, you cannot evaluate tendons and ligaments,” she says. “MRI opened the door for a whole range of new injury diagnoses allowing specific target therapies.” Garrett concurs.
“With the MRI, we obtain detailed information about an entire region,” she explains. “Deep digital flexor tendon tears, navicular bone inflammation, bone bruising, and coffin joint arthritis have different treatments and prognoses. We can diagnose and treat each more specifically and hopefully have better outcomes.”
Bone Scans and PET Scans
Nuclear scintigraphy (bone scan) employs radioactive isotopes, which, when injected, emit radioactive gamma rays. A special camera documents two-dimensional images of skeletal anatomy, showing areas with increased metabolic activity.

Reactive sites light up as “hot spots” to identify sources of lameness or other injuries. Evaluating a tissue’s physiology or what is occurring inside the tissue distinguishes the bone scan from other methods.
Scintigraphy, according to Puchalski, allows a clinician not only to identify sites that may not be clinically evident but provides an opportunity to use disease-modifying agents earlier.
“Hock arthritis shows up on scintigraphy early,” she says. “Scintigraphy also allows us to evaluate the neck, back and pelvis. A higher degree of radioactivity in an area means more active bone turnover, inflammation or injury.”
Mathieu Spriet, DVM, M.S., Dipl. ACVR, Dipl. ECVDI, Dipl. ACVR-EDI, associate professor of Diagnostic Imaging at the University of California-Davis School of Veterinary Medicine, recalls the trajectory of equine imaging during his lifetime.

“When I was in graduate school in France, the only imaging modalities we had were X-ray and ultrasound,” he recalls. “In the last 25 years, we’ve had digital radiographs, CT and MRI. I’m excited to contribute another piece by bringing the PET to the table.”
PET scans add a new chapter to nuclear medicine imaging. A radioactive tracer injected in the horse shows activity in the bones and soft tissues at a molecular level by detecting “hot spots” that illuminate injury, functional change, or inflammation on images.
The defining concept of the PET scan is the distinction between functional versus structural imaging.
“With most imaging, you are looking at the size and shape of structures,” says Spriet. “When the bone looks abnormal, it’s sometimes difficult to know if it’s abnormal because something is happening right now or if there is an old injury that is not currently active.”
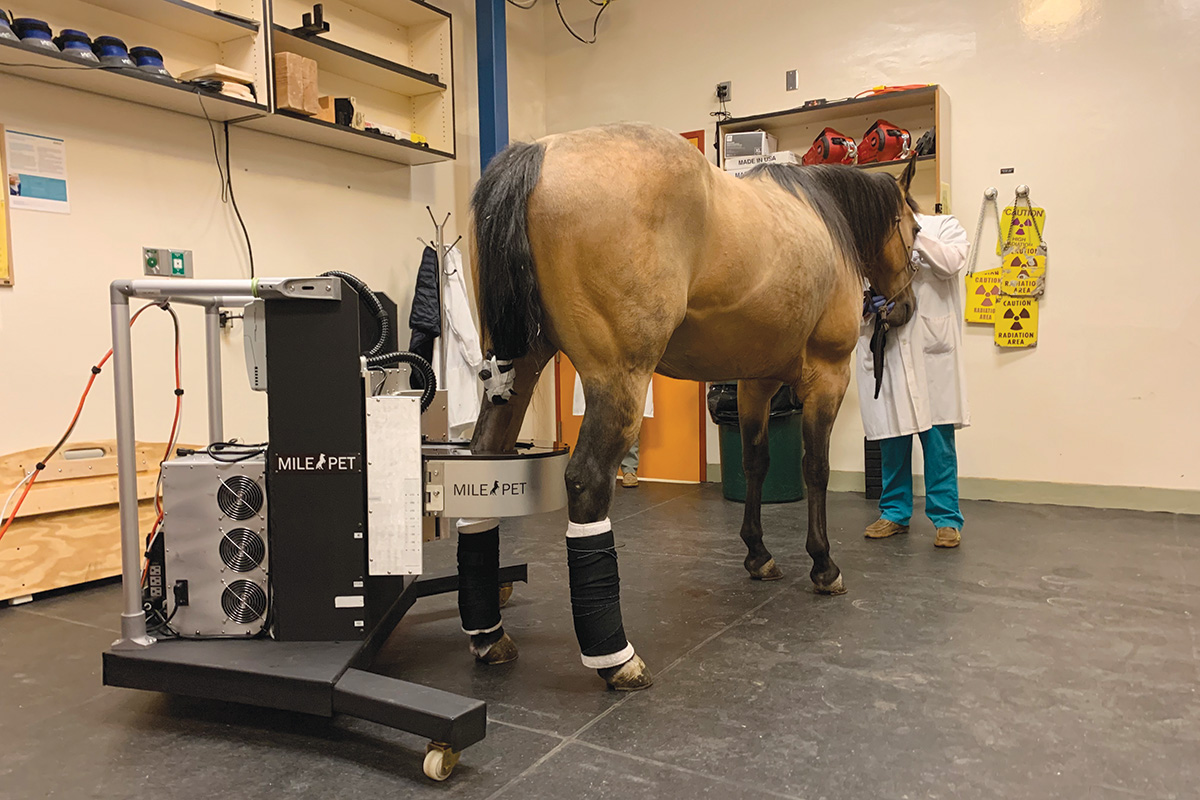
To perform the first equine PET scan in 2015, Spriet and his research team partnered with an engineering team from Maryland-based Brain Biosciences, a company specializing in state-of-the-art molecular brain imaging devices. A clinical program employing a modified human scanner imaged over 100 anesthetized horses with lameness issues.
Anesthesia carries its own level of risk to both the horse and the owner’s pocketbook. Four years after introducing the first scanner, a standing PET for a mildly sedated horse advanced this up-and-coming technology. With a standing PET, a clinician positions the horse’s hoof into an open doughnut-shaped ring before closing the apparatus around the leg. The ring’s detectors capture images from the hoof, but it can open automatically if the horse moves.
The radioactive isotope is injected 30-60 minutes prior to bringing the horse in to the room. In less than half an hour, a PET scan can image both feet and fetlocks. With an MRI scan, 45 minutes per foot or fetlock is necessary.
A Game-Changing Future
Kelly Tisher, DVM, a Colorado-based veterinarian and clinic partner at the Littleton Equine Medical Center, envisions future technology to scan a horse’s total circumference. According to Tisher, several companies are actively working to create and improve standing technology, including a robotic CT machine.
“We’ve been hoping there would be an advancement in technology to allow standing CT imaging, especially for a horse’s head and neck,” he says. “Head imaging for sinus, teeth, or other tumors is tricky. With the neck, we have an ultrasound and X-ray. Still, the ability to have 3D imaging and some sectional imaging and transverse imaging to learn about what different pathologies mean and what their clinical relevance is would be amazing.”
Each year, seeing the full picture of a horse’s anatomy to diagnose injury and disease matures. Century-old curiosity ignited a medical revolution, and today, veterinary researchers are casting light on more than a horse’s hoof.
This article about equine diagnostic imaging appeared in the January/February 2022 issue of Horse Illustrated magazine. Click here to subscribe!